68YRS WITH LEFT UPPER LOBE CONSOLIDATION ?TB WITH PLEURAL EFFUSION WITH CAD - NSTEMI WITH CKD
This is an online Elog book to discuss our patient deidentified health data shared after taking his/ her guardians signed informed consent.
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
This Elog also reflects my patient centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment
Chief complaints::
Patient daily wage worker by occupation came with c/o9390584204
FEVER SINCE 20 DAYS
COUGH since 20days
Loss of appeptite since 10days
Shortness of breath since 10 days
Weight loss since 2months
History of present illness::
Patient was apparently asypmtomatic 20 days back then she developed fever which was low grade not associated with chills and rigor ,continous not releived on medication
Cough since 20days productive scanty sputum non blood stained non foul smelling
Loss of appetite since 10 days no H/o vomitings,abdominal pain ,loose stools ,giddiness Loss of weight 5-7kgs in 4weeks
Shortness of breath since 10days insidious gradually progressive from grade 1 to 2
Left sided chest pain since 1month non radiating spasmodic type
Past History::
Known case of DM type 2 since 8yrs on medication on( insulin HAI)
Not a known case of HTN,CAD,CVD,EPILEPSY,TB,BRONCHIAL ASTHMA
Underwent S/P lap cholecystectomy (i/v/o cholelithiasis 4yrs back
Underwent S/P hysterectomy 25yrs back
Family history::
Not significant
Daily routine:: patient is a daily wage worker by occupation wakes up at 6am cooks food and has breastfast at 8am mostly jowar ghatka and goes for work mostly agricultural works and takes lunch at 1pm mostly rice with curries and at evening she takes tea at 5-6pm and cooks food for dinner and does dinner at 8pm mostly jowar roti and sleeps at 9pm.
Family history::
Not significant
Personal history::
Diet: mixed
Sleep :: adequate
Appetite:: decreased
Bowel and bladder:: regular
Addictions::Nil(occasionally takes toddy)
General examination::
After taking consent patient examined in a well lit room
Patient was conscious coherent cooperative
Well oriented to time ,place ,person
Moderate built, nourishment moderate
pallor present
No icterus
No Lymphadenopathy
No cyanosis
No clubbing
No Edema
Vitals
Temperature::99.3f
PR-110bpm
Bp-150/90 mmhg
RR--18cpm
Local examination::
Respiratory system::
Inspection::
B/L symmetrical
Trachea appears to be central
Supraclavicular and infraclavicular hallowing absent
Expansion of chest equal on both sides
No crowding of ribs
No drooping of shoulder
Wasting of muscles absent
No scoliosis ,kyphosis
No sinuses,scars,engorged veins
Palpation::
No local rise of temperature
All inspectory findings confirmed
Trachea central
Apex beat felt in 5th ICS in mid clavicular line
Percussion::
Direct : over clavicle and manubrium sternum
Indirect ::::
RT. LT .
Supraclavicular. Resonant. Resonant
Infraclavicular. Resonant. Resonanat
Mammary. Resonant. Resonant
Axillary Resonant. Resonant
Infraaxillary. Resonant Resonant
Suprascapular. Resonant. Resonant
Interscapular. Resonant Resonant
Infrascapular. Resonant Resonant
Auscultation::
B/L air entry present
On auscultation:: fine crepts heard in left upper lobe
Inspection..
Shape of abdomen...scaphoid
Umbilicus..inverted,central located
No sinuses or scars on abdomen
Palpation::
No rise in temperature
No Tenderness present
No palpable mass
No free fluid
Liver not palpable
Spleen not palpable
Percussion::
Dull note on right upper quadrant
No fluid thrill
No shifting dullness
Auscultation::
Bowel sound heard:
Cardio vascular system:
Jvp -not raised
Apex beat felt in 5th ICS in mid clavicular line
S1s2 heard
No murmurs
Central nervous system::
Speech normal
Cranial nerves intact
Sensory and motor system: normal
Reflexes.normal
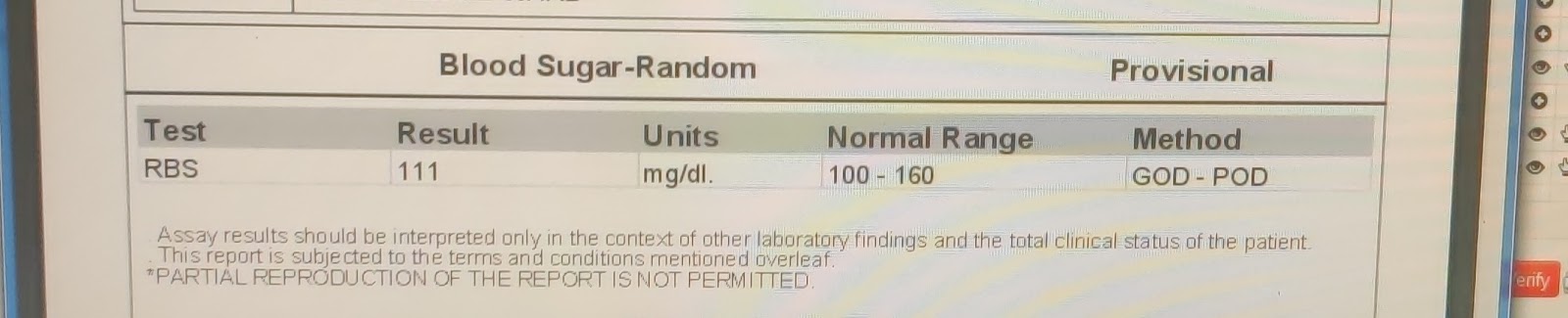
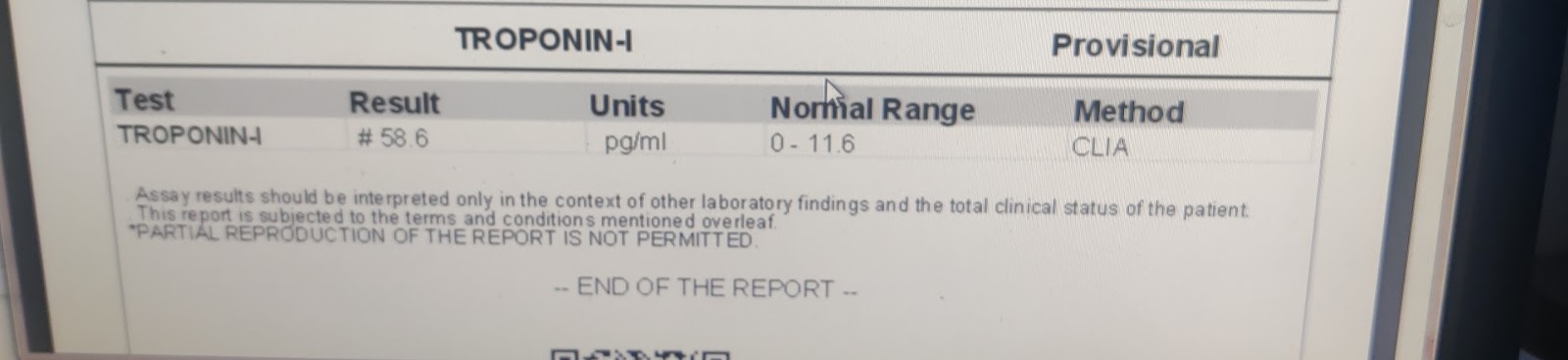
Investigations::
Chest xray PA view ::
Ecg::
2d echo::
USG ABDOMEN AND PELVIS::
Provisional dagnosis::
68YRS WITH LEFT UPPER LOBE CONSOLIDATION ?TB WITH PLEURAL EFFUSION WITH CAD - NSTEMI WITH CKD .
Treatment::
1.Tab.Ecospirin Av 75/10
2.Tab.pcm 650 mg Tid
3.syp. ascoril ls 10ml/Tid
















Comments
Post a Comment